The IVF step by step guide
We get a lot of questions asking what is the IVF treatment step by step and what does IVF look like at The Evewell, so we thought we’d take some time to break down a typical IVF cycle and explain what is unique about IVF at The Evewell.
1. The Initial Consultation
The first step of any treatment is the initial consultation, during this first consultation, you will meet your consultant who will be looking after you during your time at The Evewell. The initial consultation is a space to talk about what’s concerning you, what your family planning goals are and any questions you have regarding fertility treatment in general.
Discussing your family planning goals is something really important to consider, as this will help us plan for the future, as well as any immediate treatment.
At this meeting, we’ll go through your medical history including any previous investigations or treatment you have had. If you’ve had treatment in the past, we’ll also discuss this with you. We know that this can be upsetting but it is important that we look at this to understand what went well and what didn’t, so we’re sure we can optimise the cycle of treatment with us.
In a nutshell, this is your time to ask any questions and make sure you leave feeling fully informed and comfortable with the approach for your fertility treatment. You’ll receive a follow-up letter outlining what was discussed, any next steps (such as further investigations) and your treatment recommendations.

2. The Treatment Plan
After your Initial Consultation, your consultant will put together a bespoke treatment plan based on your medical history and your preferences for treatment.
Our goal at The Evewell is to help you achieve a successful pregnancy in the least invasive and shortest amount of time. IVF is not our default position. It may be that we can start with much less invasive treatments such as ovulation induction and IUI and this will be all that is needed. However, it may be the case that IVF is the best option based on your medical history and family planning goals.
Our Fertility Coordinator will contact you, once she has your treatment plan from your consultant, and go through with you the details of the plan and when you were hoping to start. She will then coordinate all your planning meetings to get you ready for your cycle and also send you detailed costings for your treatment.
Once you have the costings, we can organise a time to chat them through with you and answer any questions you may have.
Find out more about our pricing here.
3. The Nurse Consultation
Once you are happy with your Treatment Plan and costings, your first planning meeting is with one of our nursing team.
The Nurse Consultation is up to 90 minutes and it’s good if both yourself and your partner (if applicable) attend this meeting. We’ll go through all the regulatory consent forms that are required by the HFEA, page by page – ensuring you fully understand all elements of your treatment and answer any questions you may have at this stage.
The nurses will then take time to go through the exact protocol you are following – beginning to end, including when you’ll need to come and see us for scans, egg collection, procedures and medication.
This is a time for us to also really focus on the medication, as this is crucial to your treatment plan, and we want you to walk away from this consultation with a good understanding of what you are taking and how to take it. We know this can be a major worry for patients – so we will do all we can to take the stress out of it.
Diet and lifestyle advice will also be discussed as well as the option to have a counselling session. Read our articles on the fertility diet here and ways to increase fertility for women and men.
You’ll leave the session knowing what you need to do next and when you need to call to start your treatment.

The second planning meeting is with the Embryology team.
At The Evewell the embryologists are not just the scientists working away in the laboratory, they are a key part of our clinical team and are actively involved in your cycle. This meeting is a great opportunity for them to explain the role they will play in your treatment and also answer any questions you may have about specific procedures, such as ICSI and PGT-A.
4. The Embryologist Consultation
The embryologists will take time to explain exactly what happens in the lab, after your egg collection and then day by day during the embryo development.
If you’re having PGT-A, the team will explain exactly what this means, any associated risks and when and how the biopsies will be taken for PGT-A.
Find out more about our state-of-the-art lab here.

4. The Scanning Phase
Once you’ve called the nurses to confirm the start of your treatment cycle, you move to the Scanning Phase.
Your first scan is known as the ‘baseline scan’, on day 2 of your period. This is where we check the number of follicles and take a blood test to check your hormone levels.
You’ll then have another scan a few days later to see how your body is responding to the medication, and then you can expect to have scans every 2-3 days to monitor the progress of your follicles.
Blood tests will only be taken if they will add anything to the clinical picture – we don’t want our patients to pay for anything that isn’t needed!
In your average IVF / ICSI cycle, you can expect around 4-5 scans across a two-week period, with the bulk concentrated towards the end of the cycle.
Scans and blood tests are done in the morning, so we get the results back in time for our All Hands consultation in the afternoon (more on this later!)
5. Our All Hands Daily Medical Review Meetings
We have daily All Hands Medical Review Meetings between all clinical teams to review each patient in cycle, so despite having a dedicated doctor, you benefit from the wealth of knowledge of our entire team.
Attended by all consultants, the senior nursing team, senior embryologists and senior members of the patient services team, we use this time to review every patient who has been in that day for scans or blood tests.
We then discuss results, taking into consideration any previous treatments, and adjustments to treatment plans or medication will be made here.
This kind of holistic approach to your fertility treatment means every single patient benefits from all the consultant’s combined knowledge and experience in fertility and gynaecology.
The nurses will then contact you to update you on what to do until your next scan. This may be to carry on, with no change or that we are adjusting your medication. You should never worry – the nursing team don’t leave the building until everyone has been spoken to!
This process is a fantastic tool for both you and us. For us, it means we collaborate and share all our knowledge to optimise treatment for our patients. It also means that communication on your cycle runs smoothly across all teams. For you – you’ll always know that on the day of your scan you will hear from us about how things are going.
Find out more about why you should choose The Evewell here.

6. Egg collection
Roughly around 11-12 days after you start the stimulation medication, your consultant will decide at our All Hands Meeting that you are ready for your egg collection. The nursing team will email you the instructions for your egg collection. We then give you a call to go through them with you so that we can answer any questions or concerns you may have.
If for any reason you need advice out of hours, you’ll have access to our nurse’s emergency phone. This is answered 7 days a week until midnight. It is not a replacement for emergency services if you should need urgent medical attention, but it is super useful if you have any last-minute concerns about medication or instructions.
On the day of the egg collection, you’ll arrive at The Evewell and we will show you into one of our quiet rooms – designed to give you space and peace before your procedure.
The entire procedure usually takes around 20-30 minutes and you’ll be under deep sedation, so you aren’t aware of the procedure and won’t feel a thing.
After your egg collection, your consultant will confirm the number of eggs collected and the next steps.
7. Lab process – when the lab calls, and why they call (or don’t call)
After your Egg Collection, if you’re having IVF, a few hours after egg collection your eggs will be mixed with the sperm, and if you’re having ICSI, a single sperm will be injected into each mature egg.
Sometimes things can change on the day, so we’re always flexible in our approach so we can discuss the plan with you. We want to ensure that you get the very best chance of a successful outcome from your treatment cycle.
You’ll get a phone call the day after your egg collection to confirm how many of your eggs were fertilised. We’ll then call you again at your embryo transfer, normally 5 days after your egg collection. If you’re having a freeze all cycle or PGS, you’ll next hear from us on Day 5 to talk through how your embryos have developed.
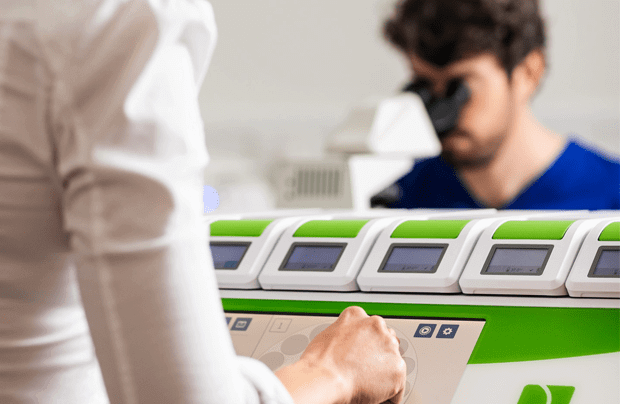
Over the next few days it may seem strange that you don’t hear from us, but rest assured we are looking after your embryos which are being observed by our time-lapse incubators. Unlike other conventional incubators, these have an integrated camera that captures images of each embryo, meaning they aren’t disturbed by constant monitoring and we have 24-hour access to their development.
9. The Embryo Transfer
After your egg collection, if you’re doing a fresh embryo transfer, you’ll start taking progesterone to prepare your lining, ready to receive an embryo, and a few days later, your embryo will be transferred into your uterus.
Your embryo transfer can be the most emotional stage of the IVF process. And it’s understandable; there is a lot riding on this moment – and it’s also the moment you’re reunited with your precious cargo.
When you arrive for your transfer you’ll be shown into one of our quiet rooms and the embryologist will then update you on the development of your embryos. They will discuss with you the embryo being transferred and potentially, whether any embryos are being frozen.
The procedure is usually no longer than 15 minutes and shouldn’t be painful, although you might experience mild cramping. It isn’t too dissimilar to a smear test. You’ll be able to go home straight after and resume a normal life.
If there is not an embryo to transfer, when you arrive you’ll meet with your consultant and the embryology team. This gives us all an opportunity to meet face to face to discuss what has happened, answer any questions and provide you with support.
10. The Two-Week Wait
Many IVF patients can find the two-week wait the hardest part of the IVF cycle. Self-care and taking it easy during the two-week wait is an important part of the process. Try to schedule some time each day to relax and unwind.
Practising things such as meditation, mindfulness, light exercise, walking or just curling up with Netflix can help during this time to help reduce stress hormones and calm the mind. Anything to help alleviate stress and anxiety! Read our full article on stress and fertility here.
We won’t want to bother you during this time – receiving a call from us can worry patients unnecessarily – but you should not hesitate to reach out to us if we can be of any support.

11. The Pregnancy test
The last part of your IVF cycle is the pregnancy test. Normally patients will want to do a home pregnancy test as soon as possible – we recommend doing this on day 12. Doing it too early may lead to unnecessary upset.
Once you have done your test, do call or email us – we are here to support you whatever the outcome and let you know the next steps. We provide full pregnancy support for patients until they are 12 weeks including blood monitoring and medications. If things haven’t worked out, we will get you booked for a complimentary meeting with your consultant as soon as possible. You will not be left on your own.
12. Counselling
Fertility treatment can be an emotional rollercoaster, so getting support from people who can relate to what you’re going through is very important.
That’s why we offer every patient a complimentary counselling session with every egg collection cycle. There are two types of counselling: supportive counselling and implications counselling.
Counselling provides individuals and couples with an opportunity to discuss their thoughts and feelings and beliefs in a confidential environment to help them see things with more clarity and gain a better understanding of the potential implications of their decisions.
Our counsellor, Gosia Heeley, is a qualified fertility counsellor, accredited by BACP (the British Association for Counselling and Psychotherapy) and BICA (the British Infertility Counselling Association).
Gosia offers face-to-face, telephone and Skype counselling sessions, with face-to-face sessions offered at two locations: The Evewell or in Guildford, Surrey.


